Digitalization in the healthcare sector offers enormous potential. But where are eHealth and mHealth applications already being used today? What opportunities do e-learning offer in medicine? And how could the transformation of the healthcare system be accomplished? In the aconium interview “5 answers”, Prof. Dr. Peter Haas, Professor of Medical Informatics at Dortmund University of Applied Sciences and Arts, explains the most important terms and the added value of digital solutions in medicine using practical examples.
aconium: In which areas are eHealth and mHealth applications already being used today?
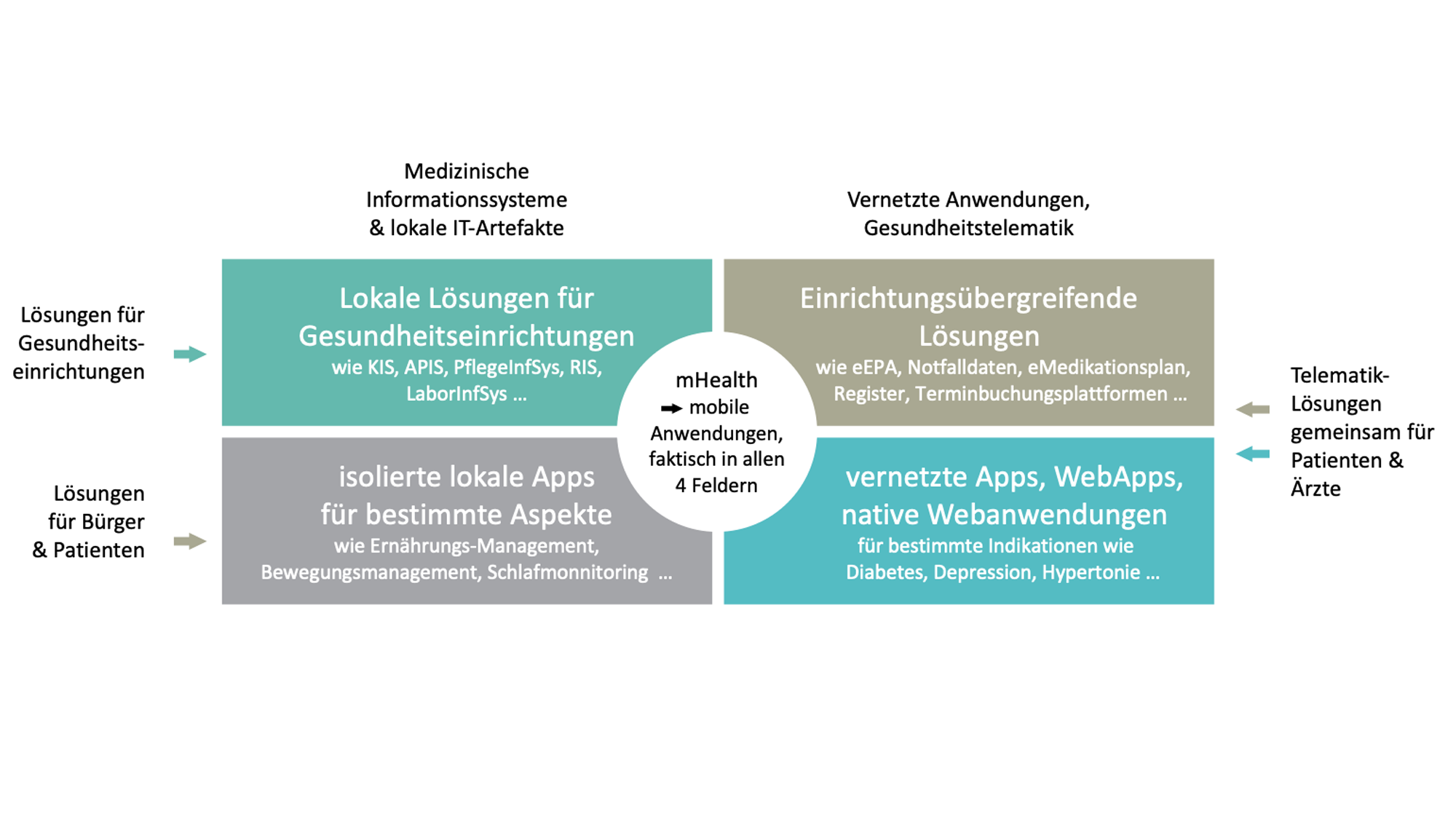
Professor Haas: First of all, we should explain what eHealth actually is, because many people equate it with telemedicine, for example. But eHealth – if you take the WHO definition, for example – encompasses much more, namely any use of information technology in the healthcare sector. This makes it clear that eHealth today permeates virtually all areas of the healthcare system. Basically, you can imagine a four-panel chart with healthcare institutions and citizens/patients vertically on the left and local applications and networked applications horizontally at the top. Then in the upper left quadrant we have the locally operated systems in the institutions such as doctor’s practice, nursing and hospital information systems with all their subsystems, in the upper right quadrant all networked applications that support communication and cooperation between the institutions such as eDoctor’s letter communication, eEmergency data, eBG report, electronic patient file and the various telemedicine applications such as teleradiology, telepathology, teleintensive care. The lower left quadrant then contains the local applications for patients, i.e. PC applications or medical apps that can run purely locally. Finally, the bottom right quadrant contains networked applications for citizens and patients, such as apps that work with central servers. However, it becomes particularly interesting when applications build a bridge and connect patient applications (i.e. those in the lower two quadrants) with applications of the professional care system (i.e. those in the upper two quadrants), thus enabling data exchange or collaboration between patients and the treating institutions. One example: the hospital patient portals promoted in the Hospital Future Act. Patients should be able to upload documents, fill in medical histories and ask questions to the hospital electronically before their stay in hospital. This would also make it possible to provide brief follow-up care if necessary. And mHealth only means that applications can also be used on the move – this could be the tablet application for the nurse in the hospital or the outpatient care service or the nutrition app for the patient.
aconium: What other opportunities does the digitalization of healthcare open up?
Professor Haas: Basically, it’s about transforming the healthcare system into an effective, highly cooperative and participatory ecosystem in which the patients themselves – insofar as they can and want to – and/or their relatives become actors, i.e. members of their own treatment team. The basis for such a healthcare system should be EHR-based treatment management platforms, as I described in the study for the Bertelsmann Foundation. Overall, however, it should not just be about digitizing the “old”, but also about new organizational and care models that exploit the potential of telemedicine, for example, and make the necessary expertise available to patients and their treatments in a timely manner. A few small examples: Every day, all surgeries deal with blood samples. Why block valuable resources? Why not set up blood collection stations where the population density makes sense, which draw blood on the basis of “prescribed” digital laboratory profiles in the patient’s EHR as a kind of commissioned service and send it to the laboratories? The attending physician then receives the laboratory report. Why not create telemedical initial consultation centers that can carry out preliminary clarifications and medical histories and thus control targeted access to care or even make visits to the doctor superfluous? Why not establish a regional digital platform for booking services and appointments so that patients don’t have to call around to get an appointment for an examination as soon as possible?
Furthermore, the value contribution of digital knowledge management is also underestimated, both within institutions and on community platforms. We now know that in no other industry is the annual growth in knowledge as great as in medicine. Timely translation also requires knowledge transfer and management platforms. But also treatment standards, process templates and many other knowledge modules. In other words, there is still huge potential in this area in the healthcare sector that is not nearly exhausted.
aconium: What do you see as challenges in the adoption of digital health technologies and how do you think these can be overcome?
Professor Haas: Let me first mention the two most important aspects that I see for eHealth applications: Benefits and usability, but these are not challenges in the true sense of the word, as they are unavoidable requirements that can in principle be easily fulfilled. In addition, however, there are real challenges, of which I believe there are four main ones: The first most important challenge is broad acceptance of digitalization in the healthcare sector among doctors, nurses, all other healthcare professionals, citizens and patients. Too often there are still reservations or data protection aspects are put forward. Of course, confidentiality and data protection must be guaranteed, that is a matter of course for me. That’s why apps that force personal health data to be stored on external servers or even do this in the background without the user’s knowledge are a no-go. And if this is necessary, it must be justified by the use case (for example, collaboration with a doctor or therapist to whom data is made available or for integration with an EHR system). And, of course, the benefits and usability of the applications must also be guaranteed for acceptance. Secondly, there is the financing of eHealth applications. After all, an important step has been taken in Germany with the possibility of an “app on prescription” for the applications in the lower two quadrants mentioned above, and the Hospital Future Act is currently funding further development in hospitals with around 4.5 billion euros. Unfortunately, however, digital innovations in outpatient care facilities remain somewhat isolated in terms of funding. Networking and collaboration are also being promoted through the national telematics platform and corresponding reimbursements. Nevertheless, it remains difficult for innovations to be sustainably funded – i.e. also for software maintenance and further development – in healthcare, for example for many applications of small spin-offs and results from university R&D projects. Thirdly, there is the standardization of important information objects and interfaces for more “open” interoperability between eHealth applications. And fourthly, there is the problem that many useful and intelligent applications will become medical devices under the new Medical Device Regulation (MDR), particularly due to Rule 11. This creates huge barriers for innovations, small innovative companies and universities that are unable to cope with the measures and costs required for MDR certification and approval. The EU has therefore made things worse here. The calculation of a score alone can now suddenly turn an entire piece of software into a medical device, even if transparency and verification of this one function and therefore patient safety would be easy to achieve.
aconium: What opportunities do you see in the use of e-learning for medical staff?
Professor Haas: eLearning was underestimated in Germany for a long time. Around 20 years ago, I introduced a course on “eLearning in medicine” into our curriculum and taught it for several years, as I was of the opinion that this would also become a professional field for medical IT specialists. But we found that hospitals and other institutions were not interested in projects and innovations and eight years ago we removed the course from the curriculum. Sadly, without the pandemic, eLearning would still not be an issue in Germany. This shows how we in Germany only act reactively when there is a need for digitalization, whereas I have hardly ever experienced proactive action with regard to digitalization in my more than 40 years of professional experience, especially in the healthcare sector. So: the opportunities of eLearning in medicine – especially in knowledge transfer but also in case-based learning – are huge, also for patient education. Multimedia, graphic simulations and interactivity create a new dimension for effective and targeted learning independent of time and space. In medicine, this can extend to training in the operation of complex devices. For eLearning in medicine in particular, I would also like to see a coordinated funding initiative from the BMG and BMBF.
aconium: What is your vision of the healthcare system of tomorrow?
Professor Haas: Even more patient-centred and individualized, scaling more precisely, more transparent, more patient-participative and more intelligent. Without sector boundaries thanks to digital collaboration between all those involved in a treatment process, with prospective planning based on a treatment management platform. In other words, easier for patients to understand, more digital and at the same time more approachable.